Type 1 Diabetes
Diabetes is a disease in which there is too much glucose (sugar) in the bloodstream. It occurs when the pancreas, a gland behind the stomach, does not produce enough insulin.
Insulin is the hormone necessary to carry sugar (produced from the foods you eat) from the bloodstream into the body’s cells, where it is used for energy. When there is not enough insulin, sugar builds up in the blood, putting people at risk for serious health problems including:
- Heart attacks and strokes
- Kidney problems
- Numbness in the feet and sores that don’t heal
- Vision problems
- Erectile dysfunction (in men)It is important to keep blood sugar lev- els as close to normal as possible to avoid the long-term complications of diabetes.
How does type 1 differ from type 2?
There are two types of diabetes—type 1 and type 2. Type 2 (also known as adult- onset diabetes) usually develops after age 40 but can sometimes appear in children, particularly if they are obese. With type 2, the pancreas produces insulin, but either there is not enough or the body can’t use it effectively. Insulin treatment isn’t always necessary, as it is with type 1.
Type 1 diabetes, also known as insulin- dependent diabetes and juvenile diabetes, can occur at any age but most often happens in children and young adults.
It is also more severe than type 2.
The causes of type 1 are not fully known. In most cases, the body’s immune system attacks and destroys the part of the pancreas that produces insulin. Family history plays a role, but only in about 10% to 15% of people with type 1 diabetes.
You are also at greater risk of developing type 1 diabetes if you have another autoimmune, hormone-related condition such as hypothyroidism, Hashimoto’s disease, or Addison’s disease.
The symptoms of type 1 diabetes can look like other conditions or medical problems. If you have these symptoms, it is important that you talk with your doctor.
Symptoms of Type 1 Diabetes
-
Increased thirst
-
Increased urination
-
Constant hunger
-
Weight loss
-
Blurred vision
-
Feeling tired all the time
How is type 1 diabetes diagnosed & treated?
Your doctor will use simple blood tests to diagnose diabetes, and to determine which type of diabetes you have and how severe it is. If your blood sugar is above 125 mg/dL before breakfast or above
200 mg/dL after eating, that may indicate diabetes. Blood sugar above 300 mg/dL can be dangerous and may need immediate attention.
A urine test for ketones is also important if you are sick (even with a mild cold) or if your diabetes is out of control (blood sugar above 300 Mg/dL). Too many ketones, which are produced when your body burns fat for energy, can mean that there is not enough insulin to move sugar from your bloodstream into your cells. If not treated, this can lead to ketoacidosis, a dangerous condition that requires immediate medical attention.
People with type 1 diabetes must have daily injections of insulin to keep a normal level of sugar in the blood. Blood sugar is kept under the best control when three or more injections per day are given, or when insulin is delivered throughout the day with an insulin pump. A healthy diet, exercise, and regular monitoring of blood sugar levels are also important to manage diabetes.
How does a person with type 1 diabetes monitor blood sugar levels?
To monitor your blood sugar, you first stick your finger or forearm with a special lancet (a needle) to get a drop of blood, which is put on a chemically-treated paper strip. Then you use a small computerized machine to read the blood sugar from the strip. Your blood sugar level shows up as a number on a screen. These blood sugar readings are used to adjust the doses of insulin that you take every day.
Your doctor or diabetes educator will discuss the various types of strips and meters that are available and prescribe one for you. They will also instruct you on how often to do this test.
What should I do with this information?
If you have symptoms or a family history of diabetes, ask your doctor if you should be tested. If you are diagnosed with diabetes, it is important that you manage your condition to avoid danger- ous long-term complications. Having diabetes requires that you take care of yourself every day. An endocrinologist, an expert in hormone-related conditions, can diagnose and treat your condition.
Type 2 Diabetes Mellitus
Diabetes is a disease caused by too little of the hormone insulin or poor use of the body’s insulin. Insulin helps your body use and store glucose (sugar) that comes from food. If insulin levels are low or not working well, sugar builds up in your blood. This causes diabetes and can lead to many problems.
In type 1 diabetes, the body cannot make insulin. In type 2 diabetes, the body does not make enough insulin
or can’t use the insulin well enough to keep the body working well. Most people with diabetes have type 2 dia- betes. Many don’t know they have it.
Type 2 diabetes is usually associated with obesity or overweight.
What are the complications of type 2 diabetes?
People with diabetes are at risk for having serious problems (complications). If your blood sugar level stays too high for too long, complications begin and can include:
- Blindness
- Kidney disease and failure
- Nerve damage and amputation(loss of toes, fingers or legs)
- Heart attack and strokeMany people can control their diabetes with diet, exercise, and medi- cations. Several types of diabetes medications help to improve blood sugar levels for people with type 2 diabetes. Some people with type 2 diabetes may have to take insulin shots so they get enough insulin.
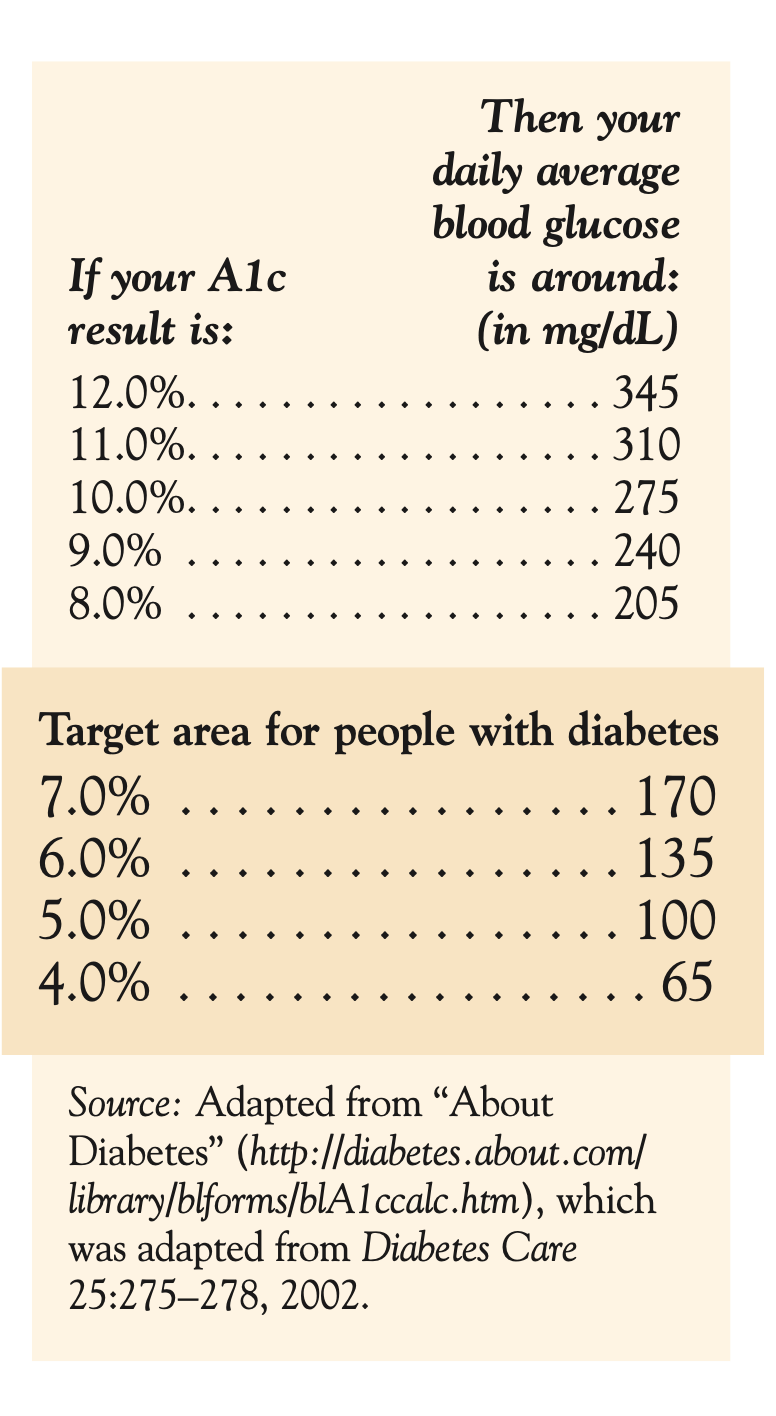
You will need to have your blood tested to learn how well you are controlling your disease. The test used to measure your control over time is the hemoglobin A1c test (A1c).
What is the difference between measuring blood sugar and A1c?
Testing for blood sugar daily tells the level of sugar in your blood at that moment. These levels change all day depending on what and when you eat, whether or not you exercise, and which medications you may be taking. A1c, however, tells information on your sugar control over the past 8 to 12 weeks.
How often should my A1c level be measured?
A1c is measured by a simple blood test performed in a laboratory. Experts recommend that you have your A1c measured four times a year. You can have the test less often if you are controlling your diabetes without medications.
People with diabetes should keep their A1c result below 7% (about 170 mg/dL or less). Studies have shown that people who keep their A1c below 7% greatly reduce their risks of developing long-term complications of diabetes. An average blood sugar for a person without diabetes is 4–6% (about 65–135 mg/dL).
What should I do with this information?
Talk with your doctor if you think you have diabetes. Share your medical and family history so you can get the best treatment. Also, adopting a healthy lifestyle that includes eating well, losing weight if needed, exercising, drinking less alcohol and not smoking will help you better manage your diabetes.