From the CDC: HRT Knowledge And Use in the United States
Why This Chartbook?
While much has been written about the risks and benefits of hormone replacement therapy (HRT), there is much less docu- mentation of its actual use in the U.S.
This chartbook offers researchers, health- care professionals, and policy makers an inventory of information available about HRT use from recent nationally represen- tative data collected by NCHS. The topics include:
The patterns of HRT use
Factors associated with HRT use
Characteristics of HRT users
The physician’s role in HRT use
Each of the NCHS surveys used include different information regarding HRT usage. Thus, the content of the survey dic- tated which data source to use to address a particular question. Because one of the surveys used collected data periodically rather than annually, use of the most recent data for each question did not result in answers that all came from the same time period.
This chartbook is not intended to be a guide on whether or not to use HRT, since that decision must be made by each indi- vidual women with help from her phy- sician. However, this overview of HRT prescription and use in the United States will be helpful to researchers and policy makers working in the arena of women’s health.
A Brief History of HRT Use
The decrease in estrogen levels in women going through menopause has interested doctors and patients for many years. Syn- thetic estrogen was developed in the 1920’s, and by the mid-1930’s it was being used to relieve menopausal symptoms. In the mid-1960’s, the book Feminine Forevertouted the use of synthetic estrogen as a way to maintain youth and femininity. This book became a hit in the lay press and greatly increased the demand for HRT.
HRTusedecreasedsharplywhenthecon- nectionbetweenuseofsyntheticestrogen andelevatedriskofendometrialcancerwas recognized in the 1970’s. Use of HRT has slowly gone up since the 1980’s, when long-term research established the protec- tive effects of HRT against osteoporosis and possibly heart disease.
Improved treatment schedules and delivery systems have increased HRT use in the U.S. To minimize the risk of endometrial cancer, physicians are much more likely to give lower doses of estrogen and to com- bine it with progesterone for women whose uteruses are intact. Furthermore, many dif- ferent formulations and dosing schedules now permit physicians to better tailor HRT to each patient.
Although we know much more about HRT today, controversy still surround its risks and benefits. Those who caution against using HRT use often cite the increased risk of endometrial and breast cancer associated with using estrogen, especially for extended lengths of time, and its common side effects such as breast tenderness, nausea, unpredictable bleeding, bloating, and mood fluctuations. Those who advocate using HRT frequently point out that HRT appears not only to alleviate menopausal symptoms, but also to reduce the risk of osteoporosis, and possibly heart disease and Alzheimer’s disease, all of which could have much greater impact than cancers on the health of postmenopausal women.
Until we have more definitive information about HRT’s effects on diseases, each woman must, with the help of her physician, weigh the risks and benefits of use. Whether or not a woman uses HRT depends on many factors: how she perceives the risks and benefits of HRT vs. the risks and potential harm of menopausal symptoms and various diseases affected by HRT; the information she obtains from her physician about HRT; and her access to health care.
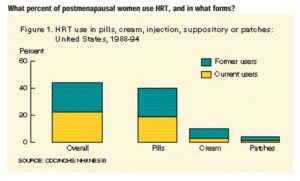
- Almost half of all postmenopausal women in the U.S. reported having ever used hormone replacement therapy (HRT). Pills were the most often used HRT preparation (Figure 1).
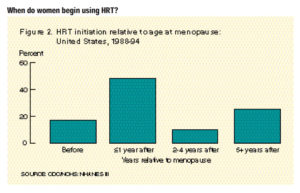
- Although most women started using HRT around the time of menopause, 25% started taking it 5 or more years after menopause (Figure 2).
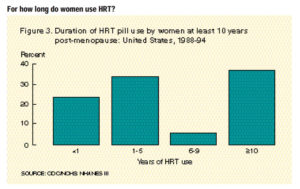
- Among women who were at least 10 years post-menopause, 14% had taken HRT pills at least 10 years (Figure 3).
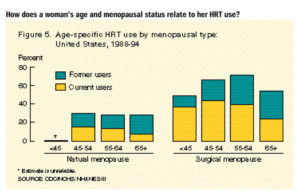
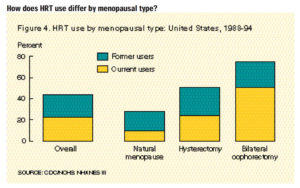
- Women with surgical menopause were much more likely to have used HRT and were more likely to be currently using it compared to women with natural menopause (Figure 4).
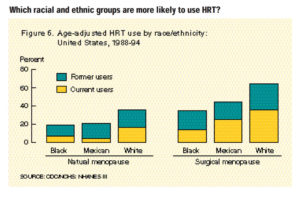
- Non-Hispanic white women were more likely to use HRT than either non-Hispanic black or Mexican American women (Chart 6).
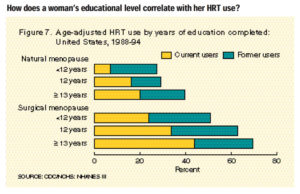
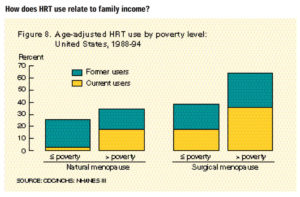
- Women with more than a high school education or whose household income was above the poverty level were more likely to use HRT than women with less education or lower family income (Charts 7 and 8).
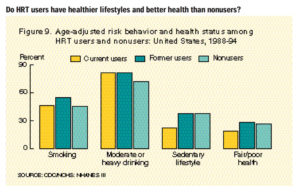
- There are no substantial differences between HRT users and nonusers in terms of risky health behaviors and self-reported health (Figure 9).
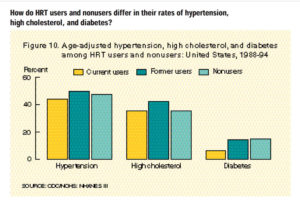
- The prevalence of diabetes was twice as high among nonusers and past HRT users than among current users (Chart 10).
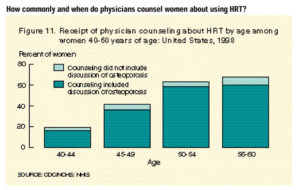
- Approximately 45% of women 40-60 years of age reported receiving counseling from a physician about the pros and cons associated with using HRT after menopause (Figure 11).
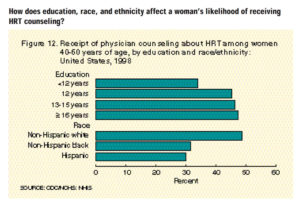
- White women were more likely to receive HRT counseling than black or Hispanic women with the same level of education;women with higher levels of education were more likely to receive counseling than women with less education, regardless of race or ethnicity (Figure 12).
-
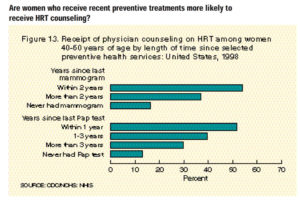
Women who had received recent preventive health services such as mammograms, Pap smears, and general examinations were much more likely to have received HRT counseling than those who had not. The more recent the services, the greater the likelihood the women had received HRT counseling (Figure 13).
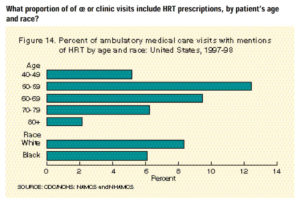
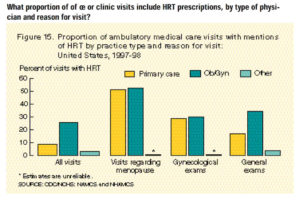
- Of all ambulatory medical care visits by women 40 years of age and over, 7.5% included an HRT prescription (Figure 14).